Access the Phase 1 Final Report: Endorsing Cost and Resource Use Measures
The Opportunity
Per capita healthcare spending in the United States are unmatched by any country in the world.1 This high rate of spending, however, has not resulted in better health for Americans. In fact, higher spending has not decreased mortality, increased patient satisfaction, or led to improvements in access or higher quality of care.2,3,4 This phenomenon of high spending with disproportionate outcomes points to a system laden with waste. The contributing factors to this concerning trend are as complex as the healthcare system itself, with physician practice patterns, regional market influences, and access to care as major drivers. Meanwhile, the United States’ healthcare spending continues to increase at a rate of seven percent per year and is largely focused on treating acute and chronic illness rather than preventive care.5 By improving efficiency, there is potential to reduce the rate of cost growth and improve the quality of care provided simultaneously. Evidence shows that not all care leads to better outcomes; thus, some portion of these current costs may be unnecessary. To identify and provide incentives for providers to deliver high quality, lower-cost care requires quality and resource use measures.
The National Quality Strategy’s (NQS) three aims—better care, affordable care, and healthy people, healthy communities—have intensified the need to identify measures that address cost and align them with the relevant quality measures already in the marketplace. The NQS specifically identifies affordability as a target area for improvement, with goals of:
- Ensuring affordable and accessible high quality health care for people, families, employers, and governments.
- Supporting and enabling communities to ensure accessible, high quality care while reducing waste and fraud.
As ongoing health reform efforts focus on expanding coverage, increasing access to care, and reducing costs, it is important to understand how resources are currently being used in the system in the context of quality, preferably related to health outcomes. Aligning resource use (or cost) and quality measures will enable the system to better evaluate efficiency of care. Several provisions in the Affordable Care Act (ACA), slated to be implemented over the next five years, require using resource use data to further support efforts to move toward a value-based purchasing (VBP) payment model. Resource use data will be included on the physician compare website, as well as a physician value modifier that will be used to adjust fee-for-service (FFS) payments by combining physician performance on quality and resources use.
In January 2010, NQF released the Measurement Framework: Evaluating Efficiency Across Patient-Focused Episodes of Care, which addressed cost and resource use as one of the three overarching domains for assessing efficiency. This framework advised that measures of resource use and cost should acknowledge the value of measuring actual prices paid, standardized prices, in addition to measuring overall utilization. Further, inappropriate care, including failing to provide an evidence-based intervention to an eligible patient or administering an intervention that is unwarranted, cannot be efficient.
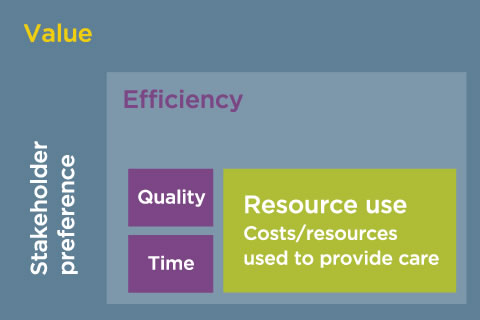
NQF’s work around endorsing cost and resource use measures has built on this concept within the Efficiency Framework report that measures of cost and quality must be aligned in order to truly understand efficiency and value (Figure 1). NQF has defined efficiency broadly as the resource use (or cost) associated with a specific level of performance with respect to the other five Institute of Medicine (IOM) aims of quality: safety, timeliness, effectiveness, equity, and patient-centeredness.
To expand the NQF portfolio of endorsed cost and resource use measures that in turn could be used as building blocks toward understanding efficiency and value, NQF embarked in 2010 on its first effort to evaluate and endorse cost and resource use measures. This learning was captured in the final reports and technical reports, yielded the first eight endorsed cost and resource use measures in the NQF portfolio, and the NQF Resource Use Measure Evaluation Criteria. Building on this work, NQF began another project to evaluate non-condition specific measures of resource use, using per-capita and per-hospitalization approaches. This work is currently ongoing. In upcoming work, NQF will continue efforts to evaluate cost and resource use measures focused cardiovascular and pulmonary conditions across two phases of work.
About the Project
For the purposes of this project, resource use measures are defined as broadly applicable and comparable measures of health services counts (in terms of units or dollars) that are applied to a population or event (broadly defined to include diagnoses, procedures, or encounters). A resource use measure counts the frequency of defined health system resources; some may further apply a dollar amount (e.g., allowable charges, paid amounts, or standardized prices) to each unit of resource use. Current approaches for measuring resource use range from broadly focused measures, such as per capita measures, which address total healthcare spending (or resource use) per person, to those with a more narrow focus, such as measures dealing with the healthcare spending or resource use of an individual procedure (e.g., a hip replacement).
This project is a three-phased effort focused on evaluating and endorsing cost and resource use measures. In the first phase, non-condition specific measures of total cost, using both per-capita or per-hospitalization episode approaches, were evaluated. Phase two will focus on cardiovascular condition specific measures and phase three will focus on pulmonary condition-specific measures.
Phase 1: Total Cost non-condition specific per capita or per hospitalization episodes
Phase 2: Cardiovascular Condition-specific per capita and condition-specific episodes
Phase 3: Pulmonary Condition-specific per capita and condition-specific episodes
Process
This project will be guided by a Steering Committee of representatives from across the spectrum of healthcare stakeholders that considers and makes recommendations regarding comments from healthcare stakeholders and existing NQF reports and prior work. Input on the clinical components of the cost and resource use measures submitted in phases two and three will be provided by clinical experts from NQF Steering Committees and/or Technical Advisory Panels (TAPs) in the specific condition areas (e.g., cardiovascular, pulmonary and diabetes). In accordance with the threes, there will be three calls for measures within the project at the start of each phase. Measures from all phases will be open for public and member comment and subsequent member voting. Candidate cost and resource use measures are being considered for NQF endorsement as national voluntary consensus standards. Agreement will be developed through NQF’s Consensus Development Process (CDP, Version 1.9).
Funding
This project is funded under NQF's contract with the Department of Health and Human Services.
For information about the availability of auxiliary aids and services for NQF’s federally funded projects, please visit: http://www.medicare.gov/about-us/nondiscrimination/nondiscrimination-notice.html.
Related NQF Work
Contact Information
For further information, contact Ashlie Wilbon at 202-783-1300 or via email at efficiency@qualityforum.org.
Notes
- Catlin A, et al., National Health Spending in 2006: A Year of Change for Prescription Drugs, Health Affairs, 2008; 27(1):14–29.
- Banks J, et al., Disease and disadvantage in the United States and in England, JAMA, 2006;295(17):2037–2045.
- Hoyert DL, et al., Annual summary of vital statistics: 2004, Pediatrics, 2006; 117(1):168–183.
- Hoyert DL, et al., Annual summary of vital statistics: 2004, Pediatrics, 2006; 117(1):168–183.
- Weiss JE, Mushinski M, International mortality rates and life expectancy: selected countries, Statistical Bulletin—Metropolitan Life Insurance Company, 1999;80(1):13–21.